Doris Obinna
When bacteria invade bone, infection occurs. This is called osteomyelitis. The bacteria eat away at the bone and damage the local blood supply, thereby preventing antibiotics from reaching the bacteria.
Infections can reach a bone by traveling through the bloodstream or spreading from nearby tissue. Osteomyelitis can also begin in the bone itself if an injury exposes the bone to germs.
In children, osteomyelitis most commonly affects the long bones of the legs and upper arm, while adults are more likely to develop osteomyelitis in the bones that make up the spine (vertebrae). People who have diabetes may develop osteomyelitis in their feet if they have foot ulcers.
Forty-four-year-old John Akpan, who suffered osteosynthesis from an open tibia fracture 10 years ago, told Daily Sun: “Months after osteosynthesis, my scar spontaneously discharged a purulent liquid while I was febrile. An implant-related infection due to Staphylococcus aureus was diagnosed. The osteosynthesis material was removed, and the underlying osteomyelitis debrided. I was given a course of antibiotic treatment with a penicillin-based agent for three months.
“Some years later, I fell down the stairs on the same place I had the infection. This time there was no fracture, but the pain did not subside despite analgesic medication for two months. With time, this pain began to be prevalent not only during exercise, but also during rest, like during the night. After 2 months into my treatment, a sinus tract developed with occasional discharge of a white-yellow liquid. This is my predicament now as I’m yet to understand this occasional discharge.”
According to experts, once considered an incurable condition, osteomyelitis can be successfully treated. Most people require surgery to remove parts of the bone that has died followed by strong antibiotics, often delivered intravenously, typically for at least six weeks.
Wilensky Nelaton probably coined the term osteomyelitis (OSM) in 1844. Bone infection, potential or actual, ever since has remained a serious clinical problem for the developing and the developed countries. Advances in understanding and control of OSM have led to the development of several classifications to guide treatment and research.
Infection of bone remains one of the most challenging problems in the field or Orthopedic Surgery. The infection can be associated with purulent drainage from a sinus tract that runs from the bone to the skin. Alternatively, bacteria may lay dormant for years, hiding within the honeycomb structure of bone and may reactivate at any time.
Osteomyelitis is often a chronic bone infection. Acute forms of bone infections are vertebral osteomyelitis, early onset or hematogenous arthroplasty infections, osteomyelitis accompanying septic arthritis, or osteomyelitis in children with a known hematogenous acquisition. Chronic forms of osteomyelitis are long bone, sacral, and foot osteomyelitis among adult patients often arising secondary to contiguous focus of infection.
Chronic osteomyelitis is often acquired by direct spread from contiguous infection that follows trauma, surgery or soft tissue ulceration (e.g., in diabetic patients or patients with neurologic disorders who are prone to decubitus). Adult patients rarely develop osteomyelitis after hematogenous seeding of long bones during bacteremia.
An Orthopedic Surgeon, Dr. Gabrield Adejimi, said osteomyelitis is an infection of the bone, a rare but serious condition. According to him, bones can become infected in a number of ways: Infection in one part of the body may spread through the bloodstream into the bone, or an open fracture or surgery may expose the bone to infection.
He said: “Only two out of every 10,000 people get osteomyelitis. The condition affects children and adults, although in different ways. Untreated bacterial like staphylococcus aureus could lead to an infection of the bone called osteomyelitis. Staphylococcus aureus is a gram-positive, round-shape bacterium that is a member of the firmicutes, and is frequently found in the nose, respiratory tract, and on the skin.
“Bone surgery, including hip and knee replacements, also increase the chance of bone infection. Only two out of every 10,000 people get Osteomyelitis. Certain conditions and behaviours that weaken the immune system increase a person’s risk for Osteomyelitis. In children, osteomyelitis is usually acute and it comes on quickly, is easier to treat, and, overall, turns out better than chronic osteomyelitis.
“In adults, osteomyelitis can be either acute or chronic; people with diabetes, HIV, or peripheral vascular disease are more prone to chronic osteomyelitis, which persists or recurs, despite treatment.
“Chronic or acute osteomyeitis often affects an adult’s pelvis or vertebrae of the spine, it can also occur in the feet, especially in a person with diabetes. Acute osteomyelitis, on the other hand, develops rapidly over a period of seven to 10 days.”
The specialists said infection has several stages, from mild to severe. According to him, mild infection does not weaken the structural integrity of the bone and allows safe use of the bone for weight bearing, but severe infection eats away at the structural integrity of the bone. When the bone loses its structural integrity, it cannot support weight and will likely break, he said.
Causes
Research states that most bone infection are caused by staphylococcus bacteria, a type of germ commonly found on the skin or in the nose of even healthy individuals. Bone infection occurs when the bacteria invade bone, either through the bloodstream or by contact with the outside environment, usually from an open fracture or surgery.
Germs can enter a bone in a variety of ways, including:
Via the bloodstream: Germs in other parts of your body, for example, from pneumonia or a urinary tract infection, can travel through your bloodstream to a weakened spot in a bone. In children, osteomyelitis most commonly occurs in the softer areas, called growth plates, at either end of the long bones of the arms and legs.
From a nearby infection: Severe puncture wounds can carry germs deep inside your body. If such an injury becomes infected, the germs can spread into a nearby bone.
Direct contamination: This may occur if you have broken a bone so severely that part of it is sticking out through your skin. Direct contamination can also occur during surgeries to replace joints or repair fractures.
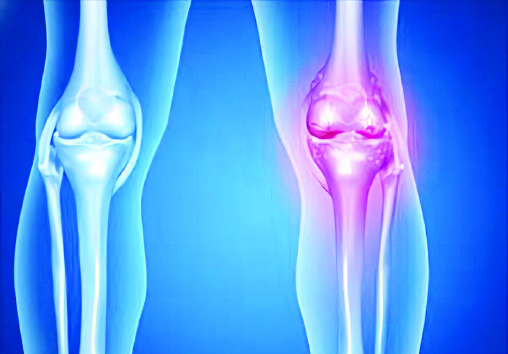
How avascular necrosis could occur
Avascular necrosis occurs when blood flow to a bone is interrupted or reduced. Reduced blood supply can be caused by:
Joint or bone trauma: An injury, such as a dislocated joint, might damage nearby blood vessels. Cancer treatments involving radiation also can weaken bone and harm blood vessels.
Fatty deposits in blood vessels: The fat (lipids) can block small blood vessels, reducing the blood flow that feeds bones.
Certain diseases: Medical conditions, such as sickle cell anemia and Gaucher’s disease, also can cause diminished blood flow to bone.
However, for about 25 per cent of people with avascular necrosis, the cause of interrupted blood flow is unknown.
Symptoms
Adejimi said the symptoms for acute and chronic osteomyelitis are similar. “They include fever, irritability, fatigue nausea tenderness, redness, warmth in the area of the infection, swelling around the affected bone and lot range of motion,” he said.
According to him, osteomyelitis in the vertebrae makes itself known through severe back pain, especially at night. He said a bone biopsy is necessary to confirm a diagnosis of osteomyelitis. This also helps determine the type of organism, typically bacteria causing the infection, so that the right medication can be prescribed.
A study shows that many people have no symptoms in the early stages of avascular necrosis. As the condition worsens, your affected joint may hurt only when you put weight on it. Eventually, the joint may hurt even when you’re lying down.
Pain can be mild or severe and usually develops gradually. Pain associated with avascular necrosis of the hip may be focused in the groin, thigh or buttock. The areas likely to be affected are the shoulders, knee, hand and foot.
Some people develop avascular necrosis bilaterally, for example, in both hips or in both knees.
Test and diagnosis
Your doctor may order a combination of tests and procedures to diagnose osteomyelitis and to determine which germ is causing the infection. Blood tests may reveal elevated levels of white blood cells and other factors that may indicate that your body is fighting an infection. If your osteomyelitis was caused by an infection in the blood, tests may reveal what germs are to blame. No blood test exists that tells your doctor whether you do or do not have osteomyelitis. However, blood tests do give clues that your doctor uses to decide what further tests and procedures you may need.
Imaging tests
X-rays: X-rays can reveal damage to your bone. However, damage may not be visible until osteomyelitis has been present for several weeks. More detailed imaging tests may be necessary if your osteomyelitis has developed more recently.
Computerised tomography (CT) scan: A CT scan combines X-ray images taken from many different angles, creating detailed cross-sectional views of a person’s internal structures.
Magnetic Resonance Imaging (MRI): Using radio waves and a strong magnetic field, MRIs can produce exceptionally detailed images of bones and the soft tissues that surround them.
Bone biopsy
A bone biopsy is the gold standard for diagnosing osteomyelitis, because it can also reveal what particular type of germ has infected your bone. Knowing the type of germ allows your doctor to choose an antibiotic that works particularly well for that type of infection.
An open biopsy requires anesthesia and surgery to access the bone. In some situations, a surgeon inserts a long needle through your skin and into your bone to take a biopsy. This procedure requires local anesthetics to numb the area where the needle is inserted. X-ray or other imaging scans may be used for guidance.
Treatment and drugs
Dr. Adejimi said treatment focuses on stopping infection in its tracts and preserving as much function as possible. “Antibiotics also help to bring the infection under control and often make it possible to avoid surgery; people with osteomyelitis usually get antibiotics for several weeks,” he said.
Also, a specialist at the International Center for Limb Lengthening, Dr. Janet Conway, said most common treatments for osteomyelitis are antibiotics and surgery to remove portions of bone that are infected or dead.
The antibiotics are usually administered through a vein in your arm for at least four to six weeks. Side effects may include nausea, vomiting and diarrhea. An additional course of oral antibiotics may also be needed for more-serious infections.
Depending on the severity of the infection, osteomyelitis surgery may include one or more of the following procedures:
Drain the infected area: Opening up the area around your infected bone allows your surgeon to drain any pus or fluid that has accumulated in response to the infection.
Remove diseased bone and tissue: In a procedure called debridement, the surgeon removes as much of the diseased bone as possible, taking a small margin of healthy bone to ensure that all the infected areas have been removed. Surrounding tissue that shows signs of infection also may be removed.
Restore blood flow to the bone: Your surgeon may fill any empty space left by the debridement procedure with a piece of bone or other tissue, such as skin or muscle, from another part of your body. Sometimes temporary fillers are placed in the pocket until you’re healthy enough to undergo a bone graft or tissue graft. The graft helps your body repair damaged blood vessels and form new bone.
Remove any foreign objects: In some cases, foreign objects, such as surgical plates or screws placed during a previous surgery, may have to be removed.
Amputate the limb: As a last resort, surgeons may amputate the affected limb to stop the infection from spreading further.
Hyperbaric oxygen therapy
In people with very difficult-to-treat osteomyelitis, hyperbaric oxygen therapy may help get more oxygen to the bone and promote healing. Hyperbaric oxygen therapy is a means of delivering more oxygen than is normally available in the atmosphere. This is done using a pressure chamber that resembles a large, clear tube.
An expert said antibiotics, alone, are rarely curative. Treatment consists of surgical debridement (removal) of infected and non-viable bone, high dose local antimicrobial therapy via antibiotic beads, intravenous antibiotics and soft tissue reconstruction as needed. Bon reconstruction is indicated in cases requiring complete removal of a section of structural bone.
“With proper treatment, even the most longstanding cases of bone infection can be cured and the patient’s quality of life can be substantially improved or returned to normal. Because of the complex nature of this area of orthopedics, choosing a surgeon who has vast experience treating bone infections is extremely important,” added an expert.
Prevention and home remedies
The best way to prevent osteomyelitis, according to Adejimi, is to keep things clean. If you or your child has a cut, especially a deep cut, wash it completely. He said: “Flush out any open wound running water for five minutes, then, bandage it in sterile bandages.”
While urging people with the infection to seek medical attention as soon as possible, he noted that the sooner you treat osteomyelitis, the better.
For acute osteomyelitis, he said early treatment prevents the condition from becoming a chronic problem that requires ongoing treatment.
“If you have been told that you have an increased risk of infection, talk to your doctor about ways to prevent infections from occurring. Reducing your risk of infection will also reduce your risk of developing osteomyelitis. In general, take precautions to avoid cuts and scrapes, which give germs easy access to your body. If you do get any cuts and scrapes, clean the area immediately and apply a clean bandage. Check wounds frequently for signs of infection,” he said.
Complications
Bone infection complications may include:
Bone death (osteonecrosis): An infection in your bone can impede blood circulation within the bone, leading to bone death. Your bone can heal after surgery to remove small sections of dead bone. If a large section of your bone has died, however, you may need to have that limb amputated to prevent spread of the infection.
Septic arthritis: In some cases, infection within bones can spread into a nearby joint.
Impaired growth: In children, the most common location for osteomyelitis is in the softer areas, called growth plates, at either end of the long bones of the arms and legs. Normal growth may be interrupted in infected bones.
Skin cancer: If your osteomyelitis has resulted in an open sore that is draining pus, the surrounding skin is at higher risk of developing squamous cell cancer.